Physiotherapy in Stroke Rehabilitation ‘Rehabilitation Phase’
Introduction
During the ‘rehabilitation phase’, the main aim for the patient is to undergo treatment to maximize movement related ability/ function. The physiotherapist aims to achieve this by delivering interventions that aim to reduce impairments and disability. (Connell, Busse, & Lennon, 2009)
In this article we will discuss the various interventions that are used by physiotherapists to improve function, reduce disability and improve mobility in stroke patients.
General Framework
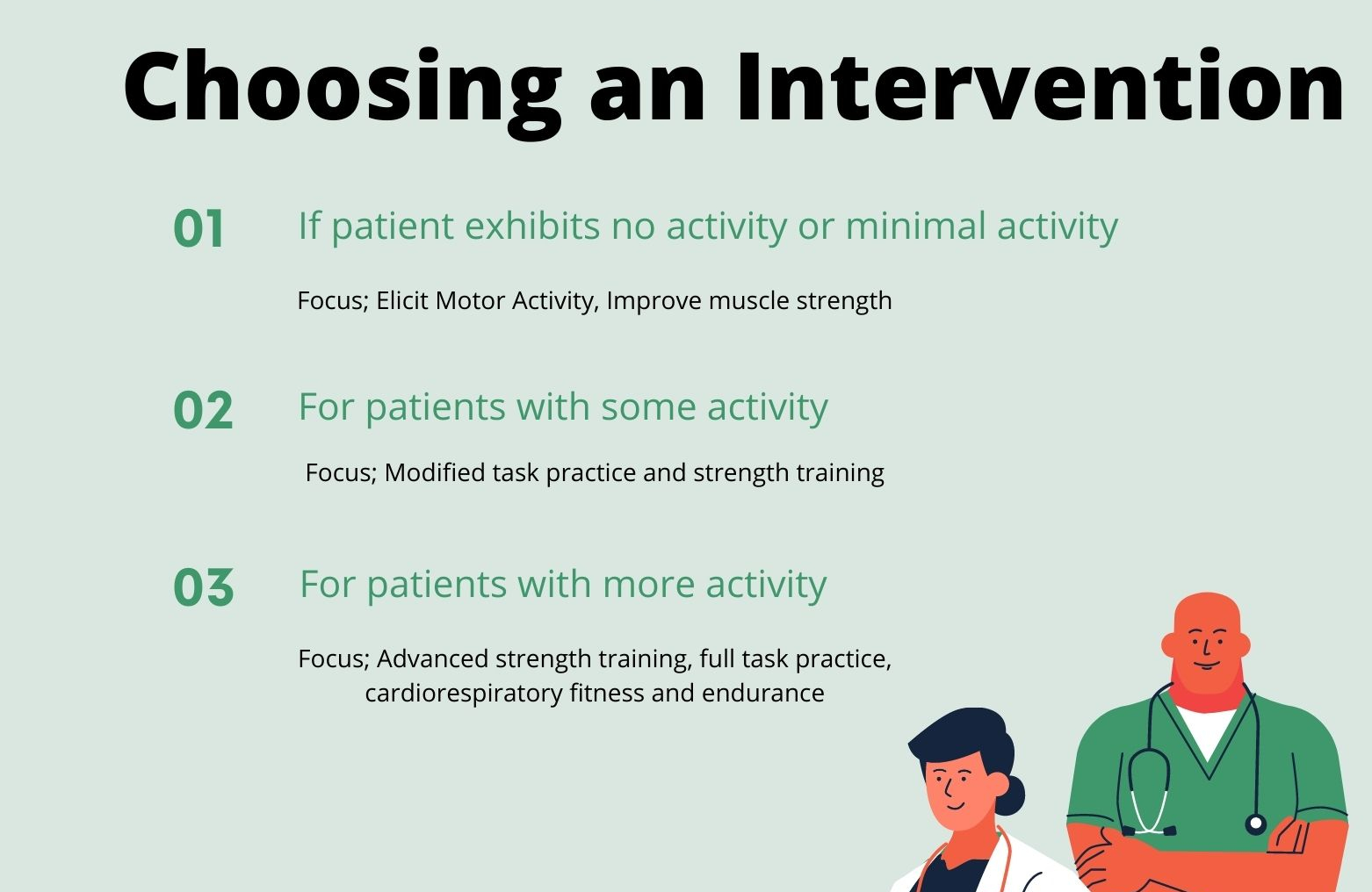
The treatment interventions that the physiotherapist starts with will essentially depend on the patient’s starting level of motor activity.(Kilbride & Cassidy, 2009)
- If patient exhibits no activity or minimal activity
Aim: Elicit Motor Activity, Improve muscle strength
- Modify exercises so that small muscle activity can lead to movement
- Eliminate gravity
- Focus on the strong mid-range activity
- Reduce friction
- Activation of the extensor activity, weight bearing through standing and sitting, treadmill training with body weight support.
- Other secondary treatments that aid in eliciting motor activity include, selective electrical stimulation, Electromyogram, biofeedback and mental practice.
- For patients with some activity
Aim: Focus on modified task practice and strength training
- Strength training through full range and inner range, increase speed, add resistance
- Task-specific training (part or modified)
- Consider adjuncts:
- FES for foot drop,
- ankle foot orthoses,
- treadmill training
- Consider rehabilitation environment and conditions for practice
- For patients with more activity;
Focus; Advanced strength training, full task practice, cardiorespiratory fitness and endurance
- Resistance training
- Body weight
- Free weights
- TheraBand
- Whole task training, lying to sitting, sit to stand, gait reeducation, reach and grasp.
- Consider the environment
- Cardiorespiratory training, walking, stepping, static, cycle ergometer, treadmill training
Improving balance.
Balance depends on sensory inputs from the visual, vestibular, and somatosensory systems. These sensory inputs are integrated and used to control anticipatory and reactive motor output to postural disturbances. (Winstein et al., 2016)
Improving sitting balance.
- Trunk training (Criekinge et al., 2019)
Strong evidence supports trunk training for improving dynamic trunk control and sitting balance. Improvements were assessed using the Trunk Impairment scale.
The trunk training involved trunk exercises or other activities targeting the trunk while sitting/lying, to minimize the influence of lower extremity function.
Exercises involved in the trunk training can be performed either on a stable or unstable surface and had to include:
- Reaching: performed beyond arm’s length to enhance the truncal influence.
- Core stability: consisting of task-specific movements of the upper and lower parts of the trunk both in the supine and sitting, for example, bridging, dead bug position, planking and so on.
- Weight shifting: the pelvis shifted the body weight to the paretic side and back, aiming to encourage the experience of weight-bearing on the paretic side during sitting.
- Sitting balance training.
Training of sitting balance while reaching beyond arm’s length results to significant improvements in sitting balance. (Veerbeek et al., 2014)
Outcome measure for assessing trunk control and sitting balance
- Trunk impairment scale
- Trunk control test
- Brunel balance assessment
standing balance
- Trunk training
Trunk training led to significant improvements in standing balance as assessed using the berg balance scale. (Criekinge et al., 2019)
- Lower limb strengthening exercises
Outcome measures
Berg Balance Scale
Four Test Balance Scale
Brunel Balance Assessment standing subscale
Romberg test
Improving upper extremity activity
Use of upper extremity is useful in daily life and its disability can lead to lack of independence in ADLs and instrumental ADLs.
- Task specific training/Functional task practice.
It’s based on the principle that practice of an action results in improved performance of that action and is focused on learning or relearning a motor skill. Key elements of task-specific training are repeated, challenging practice of functional, goal-oriented activities. All individuals with stroke should receive ADL training tailored to individual needs and eventual discharge setting.
- Constraint induced movement therapy CIMT
CIMT has been demonstrated to improve upper extremity activity, participation, and quality of life in individuals with baseline ability to control wrist and finger extension compared with usual care. (Winstein et al., 2016) (Veerbeek et al., 2014)
CIMT can be delivered in its original form, 3 to 6 hours/day for 5 days/week for 2 weeks or in a modified version 1 hour/day for 3 days/week for 10 weeks.
- Bilateral upper limb training
Moderate-quality evidence indicates that unilateral arm training (exercise for the affected arm) may be more effective than bilateral arm training (doing the same exercise with both arms at the same time). (Pollock et al., 2014)
- Robotic therapy
For the patients with severe paresis on the upper extremity.
- Mirror Therapy
Moderate quality evidence supporting the use of mirror therapy to improve upper limb function.(Pollock et al., 2014)
- NMES (neuromuscular electrical stimulation)
NMES can be used for those with minimal ability for volitional muscle activation. It may be beneficial for improving upper extremity activity if used in combination with task- specific training, particularly when applied to the wrist and hand muscles. (Winstein et al., 2016)
NMES for wrist and finger flexors resulted to significant positive effects in motor function of the paretic arm and arm – hand activities and well as in range of motion. (Veerbeek et al., 2014)
- Mental practice with motor imagery.
Useful as an addition to upper extremity exercise therapies. Longer durations of mental practice appear to produce more benefits. Mental practice of motor actions and/or activities led to improved performance of arm-hand activities. (Veerbeek et al., 2014)
- Virtual Reality and Video Games
Virtual reality and video gaming have the potential to increase participant engagement and the amount of upper extremity movement practice. And has positive effects in basic ADL performance. (Veerbeek et al., 2014)
- Somatosensory stimulation
Interventions aimed at improving somatosensory functions led to significant positive somatosensory and muscle tone. (Veerbeek et al., 2014)
Improving Mobility
- Trunk training
Trunk training led to significant improvements as assessed using the Tinetti gait subscale and the timed up and go test. (Criekinge et al., 2019)
- Circuit class therapy
Supervised circuit class training focused on gait and mobility- related functions and activities, in which patients train in groups in various work stations has positive effects for walking distance, balance, walking ability, and physical activity. (Veerbeek et al., 2014)
A 2009 meta-analysis and systematic review concluded that circuit class therapy was a safe and effective method for improving mobility after stroke. (Wevers et al 2009).
- TENS
Tens for the paretic limb has positive effects for muscle strength and walking ability. Effectiveness of TENS in conjunction with everyday activities for improving mobility, lower extremity strength, and gait speed is uncertain. (Winstein et al., 2016)
- Intensive, repetitive, walking mobility- task training.
Tailored repetitive practice of walking (or components of walking) should be practiced as often as possible for individuals with difficulty.
- Ankle foot orthosis for remediable gait impairments i.e. foot drop
- Cardiorespiratory exercise plus strengthening interventions.
- Walking training, either on treadmill or overground effective when combined with conventional rehabilitation.
- Virtual reality
- Robotics
- The effectiveness of neurophysiological approaches (ie, neurodevelopmental therapy, proprioceptive neuromuscular facilitation) compared with other treatment approaches for motor retraining after an acute stroke has not been established. (Winstein et al., 2016)
Prevention and Management of Complications
Prevention of skin breakdown and contractures (Winstein et al., 2016)
- Regular skin assessments are recommended with objective scales of risk such as the Braden scale.
- Minimizing or eliminating friction, minimizing pressure, providing appropriate support surfaces, avoiding excessive moisture, and maintaining adequate nutrition and hydration.
- Regular turning (at least every 2 hours), good hygiene, and the use of special mattresses and proper wheelchair seating to prevent skin injury.
- Daily stretching of the hemiplegic limbs to avoid contractures, and patients and families should be taught proper stretching techniques to avoid injury and to maximize effectiveness
- Positioning of the hemiplegic shoulder in maximum external rotation for 30 minutes each day either in bed or in a chair can be useful for preventing shoulder contracture
- For non-ambulatory patients, the use of a resting ankle splint at night, set in the plantigrade position (ankle at 90° and subtalar neutral) or standing on a tilt table for 30 mins/day in order to prevent contractures
Bladder incontinence
- Assessment of cognitive awareness of need to void or having voided.
- Pelvic floor muscle training (after discharge home)
- Prompted voiding
Preventing DVT.
- Mobilization
- Elastic compression stockings had an increase in skin complications and were not associated with any positive effects in reducing incidence of deep venous thrombosis (DVT) (Winstein et al., 2016)
Hemiplegic shoulder Pain
The development of shoulder pain after stroke is associated with shoulder subluxation and motor weakness. Hemiplegic shoulder pain is often multifactorial and can be associated with shoulder tissue injury, abnormal joint mechanics and central nociceptive hypersensitivity. (Winstein et al., 2016)
To prevent;
- Patient and family education (ie, range of motion, positioning) is recommended for shoulder pain and shoulder care after stroke, particularly before discharge or transitions in care
- Proper positioning.
- Maintenance of shoulder range of motion, and motor retraining.
- For people in wheelchairs, lap trays and arm troughs might be useful positioning devices to reduce shoulder pain and subluxation.
- Aggressive ROM of the shoulder if done improperly could lead to subluxation and pain.
- Avoid overhead pulleys.
Management;
- Strapping (or taping) techniques led to reduced pain outcomes as measured using the Visual Analogue Scale. (Pandian et.al. 2013) (however change was not clinically significant)
- NMES may be considered (surface or intramuscular) for shoulder pain.
Prevention of falls
- The Berg Balance Scale has demonstrated good sensitivity and specificity in predicting falls in individuals with stroke
- A community-based progressive group exercise program that includes walking and strength and balance training for 1 hour 3 times a week for participants with mild to moderate hemiparesis.
- Individuals with stroke and their caregivers receive information targeted to home and environmental modifications designed to reduce falls.
Depression
Exercise appeared to have a small beneficial effect on depressive symptoms across both the subacute and chronic stages of stroke recovery, but these effects were not retained after the exercise was terminated. 236
Winstein et al., (2016) recommends;
- Patient education about stroke is recommended. Patients should be provided with information, advice, and the opportunity to talk about the impact of the illness on their lives.
- An exercise program of at least 4 weeks duration may be considered as a complementary treatment for poststroke depression.
Poststroke Osteoporosis
Bone mass density (BMD) and lean tissue mass can reduce in both limbs after stroke. However, changes on the paretic side are more profound. BMD can decrease by >10% in <1 year in the paretic lower limb. (Beaupre et.al 2006)
This combined with the increased risk of falls greatly increases the risk of fractures.
Winstein et al., (2016) recommends increased levels of physical activity are to reduce the risk and severity of poststroke osteoporosis.
Adaptive Equipment, Orthotics And Wheel Chairs
Many patients require assistive devices, adaptive equipment, mobility aids, wheelchairs, and orthoses to maximize independent functioning after stroke.
- Single-point cane
Has one point of contact and provides a limited improvement in balance and stability.
- Tripod and quad cane
Has 3 or 4 points of contact and offer more stability. However, they are heavier, bulkier and awkward to use.
A quad cane has been shown to reduce postural sway more than a single-point cane in patients with stroke. (Laufer, 2002)
- Two-wheeled walkers, 4-wheeled walkers, or rollators.
Require the use of both arms and legs.
Support more body weight than a cane and are more energy efficient
Cannot be used on stairs.
They should be lightweight and foldable for use outside the home. Four-wheeled walkers may require hand-motor coordination to manage handbrakes on a downhill slope
- Wheel chair
Can be used for the individuals who cannot ambulate safely. The patient often propels the chair by using the less affected hand on 1 wheel and foot on the floor.
- orthotic device (an orthosis)
Ankle foot orthosis (AFOs) are commonly used by in stroke patients with lower limb motor impairments. AFOs should be used for ankle instability or dorsiflexor weakness. Other types of orthosis can also be prescribed.
Interventions that can be used in low resource settings. (Veerbeek et al., 2014)
| Function | Intervention |
| Body functions and structures | |
| Improve motor function leg | Mixed strength & Cardiorespiratory exercises High intensity practice |
| Improve motor function Arm | 1. Low – intensity modified CIMT 2. High intensity practice |
| Increasing Muscle strength (leg) | Water based exercises Strength training for the paretic leg Mixed strength and cardiorespiratory exercises High intensity exercise |
| Increasing Muscle strength (arm) | High intensity training |
| Reduce Muscle tone leg | Strength training paretic limb High intensity practice |
| Reduce Muscle tone arm | Interventions for somatosensory functions High intensity practice |
| Shoulder abduction | Passive range of motion exercises the |
| Improve gait speed | Mixed strength and cardiorespiratory exercises High intensity practice |
| Increase walking distance | Circuit class training Mixed strength and cardiorespiratory exercises |
| Reduce spatiotemporal gait patterns | Strength training of the paretic limb |
| Reduce postural sway | Standing balance training with biofeedback |
| Increase aerobic capacity | Mixed strength and cardiorespiratory exercises Cardiorespiratory exercises |
| Improve respiratory functions | Cardiorespiratory exercises |
| Improve Workload | Cardiorespiratory exercises |
| Reduce anxiety | Overground walking High intensity practice |
| Hand Movement time | Sitting balance training |
| Activities | |
| Improve sitting balance | Sitting balance training |
| Improve sitting and standing balance | Balance training during various activities Circuit class training Mixed strength and cardiovascular exercises High intensity practice |
| Walking ability | Circuit class training TENS |
| Arm hand activities | Original CIMT High intensity mCIMT Low intensity mCIMT Mental practice with motor imagery |
| Improve self-reported quality of arm-hand movement in daily life. | Original CIMT High intensity mCIMT Low intensity mCIMT |
| Improve Basic ADL | Balance training during various activities Low intensity mCIMT Caregiver mediated exercises High intensity practice |
| Increase physical activity | Circuit class training Mixed strength and cardio-respiratory exercises |
| Participation | |
| Quality of life | Mixed strength and cardiorespiratory exercises High Intensity practice |
| Leisure participation | Leisure therapy |
| Environmental factors | |
| Care giver strain | Caregiver mediated exercises |
Outcome Measures. (Measuring Improvement)
Impairments
Paresis/strength
- Motricity index
- Manual Muscle Testing
Tone
- Modified Ashworth Scale
Sensorimotor
- Fugl – Meyer
Activity
Upper extremity Function
- Action Research Arm Test
- Box and Block Test
Balance
- Berg Balance Test
- Functional reach Test
Mobility
- Walking Speed
- 6 – minute walk Test
- Timed Up and Go test
- Functional Ambulation Category
- Observational Gait Analysis
Participation
Self-reported Impairments
- Stroke Impact Scale which assess;
- Strength
- Mobility
- ADL
- Hand Function
References
Beaupre GS, Lew HL. Bone-density changes after stroke. Am J Phys Med Rehabil. 2006; 85:464–472. doi: 10.1097/01.phm.0000214275.69286.7a
Connell, L. A., Busse, M., & Lennon, S. (2009). What do acute stroke physiotherapists do ? An exploration of the content of therapy in the UK. (April 2017). https://doi.org/10.1177/0269215509334837
Criekinge, T. Van, Truijen, S., Schröder, J., Maebe, Z., Blanckaert, K., Waal, C. Van Der, & Vink, M. (2019). The effectiveness of trunk training on trunk control , sitting and standing balance and mobility post-stroke : a systematic review and meta-analysis. https://doi.org/10.1177/0269215519830159
Kilbride, C., & Cassidy, E. (2009). The stable acute patient with potential for recovery: stroke, TBI and GBS. In Pocketbook of Neurological Physiotherapy (p. 308). Elsevier Health Sciences.
Laufer Y. Effects of one-point and four-point canes on balance and weight distribution in patients with hemiparesis. Clin Rehabil. 2002;16:141–148
Pandian JD, Kaur P, Arora R, Vishwambaran DK, Toor G, Mathangi S, Vijaya P, Uppal A, Kaur T, Arima H. Shoulder taping reduces injury and pain in stroke patients: randomized controlled trial. Neurology. 2013;80:528–532. doi: 10.1212/WNL.0b013e318281550e.
Pollock, A., Se, F., Mc, B., Langhorne, P., Ge, M., Mehrholz, J., & F, V. W. (2014). Interventions for improving upper limb function after stroke ( Review ). (11).
Veerbeek, J. M., Wegen, E. Van, Peppen, R. Van, Wees, P. J. Van Der, Hendriks, E., Rietberg, M., & Kwakkel, G. (2014). What Is the Evidence for Physical Therapy Poststroke ? A Systematic Review and Meta-Analysis. 9(2). https://doi.org/10.1371/journal.pone.0087987
Wevers L, van de Port I, Vermue M, Mead G, Kwakkel G. Effects of task-oriented circuit class training on walking competency after stroke: a systematic review. Stroke. 2009;40:2450–2459. doi: 10.1161/ STROKEAHA.108.541946
Winstein, C. J., Stein, J., Arena, R., Bates, B., Cherney, L. R., Cramer, S. C., … Rp, A. (2016). AHA / ASA Guideline Guidelines for Adult Stroke Rehabilitation and Recovery. https://doi.org/10.1161/STR.0000000000000098