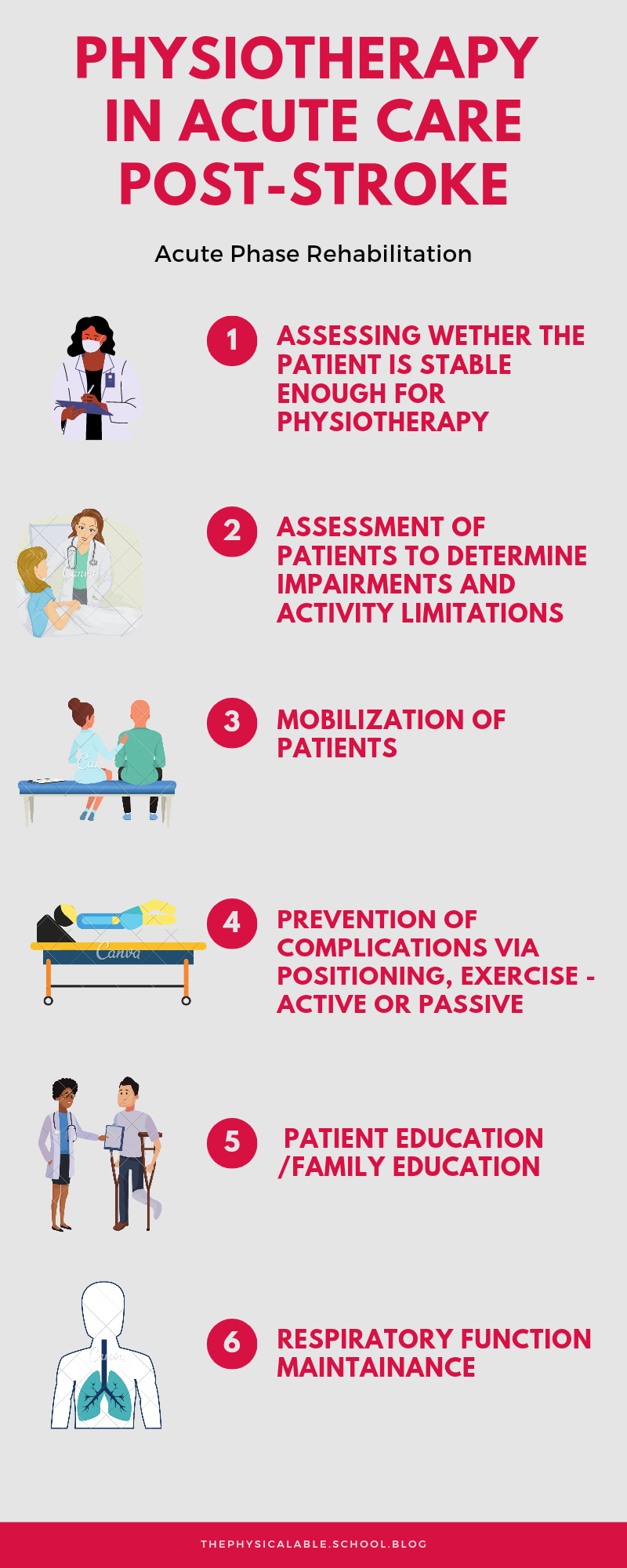
Physiotherapy in Stroke Rehabilitation ‘Acute Phase’
Introduction
The Acute/Assessment phase is the period when the physiotherapist/stroke team are primarily gathering information about the patient identifying impairments and disability, assessing the social and personal context and environment, monitoring response to treatment, etc. In most cases this would be a short-lived stage – a few days – usually following admission, either to an acute ward following the stroke, or transfer to a rehab unit. (Connell, Busse, & Lennon, 2009)
According to the American Stroke Association (ASA)/ American heart association (AHA) guidelines (Ackerson et al., 2018);
- Early rehabilitation for hospitalized stroke patients should be provided in environments with organized, interprofessional stroke care.
- A functional assessment by a clinician with expertise in rehabilitation should be performed.
- Stroke patients should receive rehabilitation at an intensity commensurate with anticipated benefit and tolerance.
- High-dose, very early mobilization within 24 hours of stroke onset should not be performed because it can reduce the odds of a favorable outcome at 3 months.
- Stroke patients should be provided with a formal assessment before discharge from acute care hospitalization and these findings should also be incorporated into the care transition as well as the discharge planning process.
This article will focus on the role played by the physiotherapists in the acute/assessment phase.
Assessing medical stability
- Medical notes
- Talking to key Members of the multidisciplinary team.
Patient Assessment
- Subjective assessment
- Objective assessment
- Motor assessment
- Sensory Assessment
- Postural Assessment
- Balance and coordination assessment
- Gait assessment
- Functional assessment
Assessment
Assessing for medical stability
Acute patients may be sedated, paralyzed and intubated with impaired levels of consciousness, they may also be conscious and be able to communicate with or without difficulty. Before deciding whether to continue it is important to determine if the patient is medically stable.
To determine whether the patient is stable;
- Talk to the key members of the medical team.
- Check the medical files/notes.
Checking the medical notes will inform you of any risk factors that might be at play. Important information to get from the medical notes will include things like;
- Type of stroke
- Planned medical management
- Risks i.e. re-bleeds or extension of stroke
- Change in neurological status over the last hours
- Other pre-existing conditions
- Cardio-vascular stability
- ABGs
- Glucose levels
- FBC results
Subjective Assessment.
The next step of your assessment will be subjective assessment. In subjective assessment the therapist gathers general information from the medical record, the various members of the multidisciplinary team (MDT) and the patient and/or family.(Kilbride & Cassidy, 2009). Information that has been obtained when assessing for medical stability will also be useful in subjective assessment. In fact, the assessment of medical stability can be said to be part of the subjective assessment.
Interviewing the patient or family
The subjective assessment interview will provide an opportunity for creation of rapport between the therapist and the patient or the family. The interview also allows the physiotherapist to observe/assess various issues such as positioning, postures, communication abilities of the patient, mental status, patient attitudes, orientation and ability to follow instructions. All these factors are relevant in stroke patients.
Important information to get from the patient/family interview includes;
- Patients biodata (name, occupation, religion, age)
- Past medical history especially history of any neurological disorders
- Comorbidities
- Drug history including (caffeine, alcohol, smoking)
- Specialized equipment that the patient was using, (glasses, hearing aid etc.)
- Physical Activity/mobility levels before the stroke
- Normal daily routine and leisure activities.
- Any history of challenges in mobility, communication, pain
- Patients/family expectation of treatment.
The other important factors to check in subjective assessment include patient complaints i.e. pain, stiffness etc.
The physiotherapist should consider certain factors such as depression and fatigue which might influence assessment.
Objective Assessment
The objective assessment consists of observation and examination; it begins with the observation of activity level and voluntary movement control. Objective assessment in the acute care will generally focus on;
- Identifying the functional activity level of the patient
- Identifying intact motor abilities
- Identification of Postural and Movement deficits.
- Identify Underlying impairments
Identifying the functional abilities of the patient.
In assessing the functional abilities of a patient, the physiotherapist will ask the patient to perform some specific movements of the trunk/limbs or to perform a task During this examination, the therapist should refrain from physically assisting the patient, but may offer verbal cues or demonstration to determine potential for improved performance.
Once the physiotherapist has established the functional abilities that the patient can perform independently and safely, he/she can further assess how much assistance the patient requires to perform other complex activities.
Functional abilities assessed can include;
- Changing position in bed (rolling, scooting etc.)
- Moving from lying to sitting
- Sitting to standing
- Sitting abilities (balance)
- Standing ability (balance)
- Walking ability.
- Bed transfers, i.e. bed to chair
Identifying intact motor abilities
Intact motor abilities refer to the motor functions that the patient can perform, i.e. Abduct left arm – gravity eliminated, Ability to flex/extend fingers left arm
Framework for Objective Assessment
Motor impairment assessment
- Muscle strength
Stroke is usually associated with loss of muscle strength in the contralateral side of the body. Assessment of this involves the use of Manual muscle testing muscle grades.
- Tone
In the early stages of stroke muscle tone might be reduced (hypotonia) then later it could be increased (hypertonia) with evidence of spasticity.
Modified ashworth scale is used to assess tone
- Rigidity
It is the increased resistance to passive movement which is constant throughout the range of movement, occurring throughout the full range of passive movement. Cog wheel or lead pipe.
- Coordination
Coordination is the ability to use different parts of the body together both smoothly and efficiently and involves the complex coordination of multiple joints and muscles. Lack of coordination suggests cerebellum involvement it is responsible for the integration the sensory motor systems to produce smooth movements.
Assessment tests include; Finger nose test, heel shin test
Sensory Impairment Assessment
- Light touch
Assessed using some light material i.e. cotton wool comparing sensation on a part of the body with the opposite one.
- Pain
Assessed using a pin or any other sharp object, comparing pain sensation on the opposite sides.
- Proprioception
Assessed using the distal proprioception test where the assessor will move joints of the hip, knee ankle and big toe up and down while the patient watches. Then ask the patient to repeat the same movement with eyes closed.
- Reflexes
Deep tendon reflexes
assessed via use of a patella hammer. In early stages, deep tendon reflexes might be diminished however after some time they are hyper reflexive (exaggerated) indicating upper motor neuron involvement.
Plantar reflex (Babinski’s sign)
Assessed via plantar stimulation
Evidenced by the dorsiflexion of the great toe with or without fanning of the other toes and withdrawal of the leg.
| Impairments | Method of Assessment |
| Hemiplegia | Sensorimotor assessment |
| Muscle Weakness | Medical Research Council (MRC) grades |
| Fatigue | Fatigue severity scale |
| Loss of dexterity | Nine-hole peg test Purdue pegboard test |
| Altered sensation | Nottingham Sensory Assessment |
| Proprioceptive loss | Distal proprioception test Finger nose finger test Reaching tests |
| Altered Tone | Modified Ashworth scale |
| Cognitive/perceptual impairments | Mini Mental Cognitive test |
| Coordination | Finger nose test |
| Visual field impairment | Snellen’s chart |
| Pain | Visual Analogue Scale |
| Swelling/Edema | Observation + tape measure |
| Emerging habitual postures | Observation |
| Decreased ROM | Goniometry |
| Cardiovascular deconditioning | Borgs rate of perceived exertion |
Posture Assessment
Posture refers to the attitude assumed by the body either when its stationary or moving. One of the most observable postures in stroke would probably be hemi spatial neglect/ Contraversive pushing.
Gait Assessment
Gait assessment involves asking the patient to walk around (i.e. 10-minute walk test) observing the different gaits cycles and the function of the lower limb while walking.
Analysis of a gait cycle will aid in assessing;
- Walking aids / orthotics
- Pattern
- Distance covered
- Speed of walking
- Attention
- Orientation
- Memory
- Cognitive status
Abnormal gait patterns that can be observed in stroke include;
During heel contact/loading phase
- Limited ankle dorsiflexion
- Lack of knee flexion
During mid stance
- Lack of proper knee extension (with excessive dorsiflexion)
- Stiffening of knee
- Limited hip extension and ankle dorsiflexion (contracture of soleus) that doesn’t propel body mass forward.
- Excessive Lateral Pelvic Shift
During late stance/ pre-swing
- No knee flexion or ankle plantar flexion which are required for push off
During early swing and mid swing
- Limited knee flexion (35 – 40 degree required for toe and swing clearance in early swing which increases to 60 degrees in mid swing)
- Toe clearance limited
During late swing
- Limited knee extension and ankle dorsiflexion which will affect heel contact and weight acceptance.
Functional assessment.
Functional assessment is vital to ensure the patient receives the level of support required on the ward and also provides assistance with goal setting and treatment plans. Specific aspects that are assessed include;
Bed Mobility
Rolling
Most patients will have difficulty rolling over to the affected side.
Assess if the patient is able to change lying position (rolling) from one side to another safely and independently. (Verbal assistance may be given) If not how much assistance is required.
Getting out of bed
Assess the ability to get out of bed independently or the amount of assistance required to do this safely.
Scooting
Assess the ability of the patient to move over while in bed, through trunk control.
Sitting at the edge of bed
Assess sitting balance and the assistance required.
Movement while sitting and how it affects i.e. reaching out beyond base of support.
Transfers
Only progress to assessing transfer once patient can easily sit at the edge of the bed easily. This minimizes risk of hospital falls.
Assess the different types of transfers while providing education to care givers on how to perform this safely. Note the amount of assistance required and the devices/postures used.
Other functional assessments that might be performed but aren’t mostly involved in the acute phase include;
- Upper Limb Function assessment
- Lower Limb Function assessment
- Mobility assessment
- Stairs
| Activity | Tools/ Measures |
| General activity | Barthel index |
| Upper limb function | Action Research Arm Test |
| Mobility; Bed rollingSleep to SitSit to stand | Trunk control test Observation (note on assistance required) |
| Transfers; Bed to chair | Observation (note on assistance required) |
| ADL | Functional independence measure |
Problem list
After assessment the next step is to create a problem list. A problem list contains all the impairments and activity limitations the patient is facing.
Hypothesis
A hypothesis tends to correlate the impairments and the activity limitations i.e. one might hypothesis that the inability of a patient to perform rolling is due to:
- Lack of trunk control/ trunk muscle weakness
- Impaired proprioception
- Paralysis of the upper and lower extremities
Hypothesis is leads to better intervention planning.
Goal setting
Generally, the overarching goal should be to improve functioning. Small specific goals should be set that works towards the main goal should be set and well defined.
Mark & Levack (2018) point out that in acute care in cases where the patient is overwhelmed by the new disorder and isn’t adjusted well enough to be involved in the creation of goals, the health care professional might take charge. In this case, the overreaching main goal will be independent mobility in three months. Goals set should be meaningful to the patient.
Other short-term specific goals might work towards this goal includes;
- Achieving bed mobility (rolling, to either side and side lying to sitting) with minimal support (less than 25% support) in 3 days
- Achieving independent bed mobility (rolling, side lying to sitting) (1 week)
- Independent balance in static sitting. (2 weeks)
- Independent sit to stand (1 month)
- Achieving assisted ambulation (walking aid or support from someone) in 1 month.
Interventions
The main aims of acute stroke physiotherapy involves (Connell et al 2009);
- Getting the patient out of bed as soon as possible
- Facilitating active participation in mobility activities (such as bed mobility, transferring from one seat to another and walking depending on the patient’s level of ability)
- Preventing complications such as loss of joint range and cardiovascular deconditioning and disuse atrophy
- Encouraging the patient to move their limbs
- Respiratory function maintenance (intubated patients)
- Patient education
Maintenance of muscle integrity and range of motion
- Passive/ active assisted range of motion exercises.
- Positioning
- Active assisted exercises.
Positioning
Positioning helps in reducing/preventing:
- Skin damage
- Limb swelling
- Shoulder pain
- Subluxation
- Discomfort
- Respiratory complications
- It also helps maximize function and maintain soft tissue length.


Positioning recommendations
Chair
- sitting in an armchair (Arm Support devices such as a Lap Tray may be used to assist with arm positioning for those at risk of shoulder subluxation)
- Chair positioning with family addressing from hemiplegic side
- Trunk positioning with blanket roll to maintain upright
- Hemiplegic arm supported on bedside table
- Legs in neutral position can use blanket roll to assist
- Feet flat on floor
Bed
- Side lying on the unaffected side then side lying on the affected side. (2 hourly turning positions)
- Elevation of the limb when resting for individuals who are immobile to prevent swelling in the hand and foot (above the heart)
- Positioning for increased stimulation of the affected side for patients with hemi spatial neglect
- Head positioning with towel roll
- Hand with wash cloth roll.
- Foot positioning with Foothold boots or Skin Care heel float or pillow for positioning
Bed mobility
Rolling over.
Sitting out of bed
Practicing reaching beyond arm’s length while sitting with supervision/assistance should be undertaken for individuals who have difficulty with sitting. Improves balance in sitting (Veerbeek et al., 2014)
When sitting out of bed:
- Address upright orientation
- Use foot stool if feet are not touching ground
- If patient is pushing or leaning to one side, you can sit next to them
- Eyes open and focusing on vertical object in front of them
Transfers



Standing
For individuals with difficulty standing:
- Practicing functional task-specific training while standing
- Walking training that includes challenge to standing balance
- Providing visual or auditory feedback
- Lower limb strengthening exercises
- Consider ankle foot orthosis
Getting the patient out of bed (Mobilization)
Early mobilization includes commencement of sitting, standing and walking training out of bed early after stroke. It helps combat the complications of immobility (bed rest) i.e. cardiovascular deconditioning, deep venous thrombosis etc.
How early is early mobilization? Verbeek et al (2014) defines early mobilization as mobilizing a patient out of bed within 24 hours after the stroke, and encouraging them to practice outside the bed.
Concerns that argue against early mobilization include; raising the patients head early after stroke will impair cerebral blood flow and cerebral perfusion or as in the case of intracerebral hemorrhage it might increase the risk of inducing further bleeding.
The AVERT RCT (A Very Early Rehabilitation Trial) compared high-dose(frequent), very early mobilization with standard-of- care mobility. Its concluded that short bursts of mobilization repeated regularly might best achieve recovery. (Langhorne et al 2017)
Respiratory function maintenance (Intubated patients/unconscious)
- Positioning
- Manual techniques (shaking, vibrations, percussions)
- Manual hyperinflation
- Suctioning.
Patient Education
Encourage them to actively use of the hemiplegic hand. If unable then utilize the normal hand to move the other hemiplegic hand. Same case with the lower limb.
In dressing advise the patients to start with the hemiparetic limb and end with it.
Encourage firm rubbing of the hemiparetic side when bathing (sensory stimulation)
Prognosis
| ADL independence | Walking | Dexterity |
|---|---|---|
| Younger age | Younger age | Initial severity of motor impairment and function, e.g. Presence of shoulder abduction and finger extension |
| Less severe neurological deficits | Less severe sensorimotor dysfunction of the paretic leg | |
| Better sitting balance | Absence of homonymous hemianopia | |
| Absence of urinary incontinence | No urinary incontinence | |
| Limited comorbidity | Adequate sitting balance | |
| Consciousness at admission | Better initial ADL function and ambulation | |
| Better cognitive status | Better level of consciousness on admission | |
| Absence of depression |
Outcome measures that can be used in Acute Stroke
Used to assess quantitatively stroke-related neurologic deficits.
It is simple, fast (5 mins) and can be administered by non-neurologists.
It is also used to measure stroke deficit
It is also brief (5 mins), valid and reliable.
The motricity index is used to quantitatively assess motor impairment.
It is a brief assessment (5 mins) of motor function of arm, leg and trunk. It has low sensitivity.
References
Ackerson, T., Adeoye, O. M., Brown, M., Demaerschalk, B. M., Hoh, B., Leslie-mazwi, T. M., … Summers, D. V. (2018). AHA / ASA Guideline 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. https://doi.org/10.1161/STR.0000000000000158
Connell, L. A., Busse, M., & Lennon, S. (2009). What do acute stroke physiotherapists do ? An exploration of the content of therapy in the UK. (April 2017). https://doi.org/10.1177/0269215509334837
Kilbride, C., & Cassidy, E. (2009). The stable acute patient with potential for recovery: stroke, TBI and GBS. In Pocketbook of Neurological Physiotherapy (p. 308). Elsevier Health Sciences.
Veerbeek, J. M., Wegen, E. Van, Peppen, R. Van, Wees, P. J. Van Der, Hendriks, E., Rietberg, M., & Kwakkel, G. (2014). What Is the Evidence for Physical Therapy Poststroke ? A Systematic Review and Meta-Analysis. 9(2). https://doi.org/10.1371/journal.pone.0087987
Ackerson, T., Adeoye, O. M., Brown, M., Demaerschalk, B. M., Hoh, B., Leslie-mazwi, T. M., … Summers, D. V. (2018). AHA / ASA Guideline 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. https://doi.org/10.1161/STR.0000000000000158
Connell, L. A., Busse, M., & Lennon, S. (2009). What do acute stroke physiotherapists do ? An exploration of the content of therapy in the UK. (April 2017). https://doi.org/10.1177/0269215509334837
Kilbride, C., & Cassidy, E. (2009). The stable acute patient with potential for recovery: stroke, TBI and GBS. In Pocketbook of Neurological Physiotherapy (p. 308). Elsevier Health Sciences.
Veerbeek, J. M., Wegen, E. Van, Peppen, R. Van, Wees, P. J. Van Der, Hendriks, E., Rietberg, M., & Kwakkel, G. (2014). What Is the Evidence for Physical Therapy Poststroke ? A Systematic Review and Meta-Analysis. 9(2). https://doi.org/10.1371/journal.pone.0087987


Pingback: Stroke Rehabilitation – Acute Phase – Physicalable